Through a grant from the Ontario Trillium Foundation and the support of the North East Local Health Integration Network the Northeastern PPMD Strategy was developed. Through the consultation and expertise of Project Director, Linda Rankin, and Community Development Coordinator, Michelle Deveau Brock, six communities in Northeastern Ontario including Nipissing, Muskoka/Parry Sound, Sudbury, Sault St. Marie, Timmins and Timinskaming came together to create a strategy to address the postal code lottery for PPMD in Ontario’s Northeast. This strategy reflects the combined voices of working groups in each community comprised of professionals, community members, women with lived experience, a PPMD PhotoVOICE project, individual interviews and a best practice literature review. Below you will find more details on the Northeastern PPMD Strategy.
Please be advised that this video depicts the true nature of those who have experienced postpartum mood disorder and may not be appropriate for all audiences.



PPMD carries with it the burden of shame, stigma and silence that further complicates the already complex.
Postpartum Mood Disorder (PPMD) is a multifaceted, gendered, political, and global issue. The etiology of PPMD varies according to the theoretical and ideological orientation of the reference source. The rhetoric remains blurred within both the literature and the medical and social welfare discourses. These factors have impacted the diagnosis and treatment of this mental health issue within Ontario and results in families becoming victims of a postal code lottery in which their access to services is dependent upon their luck in residency.
"Hopefully because of our stand they will have a place to go to get the help they need free from stigma, stereotypes, shame and fear!” - Michelle Roberts
The implications for a lack of awareness, diagnosis and treatment for this disorder can have profound effects on mothers, fathers, infants, partners and the entire family. Furthermore, PPMD carries with it the burden of shame, stigma and silence that impede access to services. Due to the complexity of the issue, which engages multiple domains including the physical and mental health of the parents, child health, child development and child welfare, it necessitates a strategic comprehensive response.
Postpartum blues occurs after the birth of a child and can affect up to 75% of mothers. It normally lasts for 10 days and mothers tend to exhibit symptoms such as crying, fatigue, irritability and anxiety, but, unlike other forms of PPMD, postpartum blues does not typically require formal intervention (Beck, 2006). PPMD often involves co-morbid presentation of anxiety and depression. Symptoms of PPMD include mood lability, irritability, insomnia or hypersomnia, obsessive thoughts, changes in appetite, tearfulness, anxiety, feelings of worthlessness, poor concentration, interpersonal hypersensitivity and loss of interest or pleasure. Postpartum post-traumatic stress disorder (PPTSD) has recently begun to receive attention within the literature. However, due to variances in concepts and methodology, accurate rates of impact are difficult to authenticate. A recent Canadian study of PPTSD has reported it affecting 7.6% to 16.6% (Verreault et al., 2012) of mothers. Postpartum psychosis, which affects approximately 1 in 1000 births (Kendell, 1987), is inclusive of symptom clusters that includes hallucinations, delusions, and extreme agitation and can also include thoughts of harm to self and to others.
Globally, we are seeing initiatives beginning to emerge that are attempting to address the complexities of PPMD. Each initiative is addressing the issues of PPMD in unique ways. However, each strategy demonstrates a commitment to addressing the issues facing families and communities that are struggling with PPMD, as well as demonstrating the importance of a systematic response to PPMD.
The call for participation with the Northeastern Ontario Postpartum Mood Disorder Project working groups was facilitated primarily through presentations to key stakeholder groups throughout Northeastern Ontario as well as through telephone and email requests. Members volunteered to join the working groups and committed to one year of involvement with the project. The Working Groups had two primary responsibilities: (1) to inform and guide the development of the Northeastern Ontario Postpartum Mood Disorder Strategy; and (2) to assist in the recruitment of women and families with lived experience of PPMD to participate in the photovoice project.
Working Groups in each of the six districts were formed and consisted of three to ten members, representing a variety of community organizations and community members with an interest (either professional or personal) in PPMD. Membership included:
Over the course of the project each working group completed a service map of PPMD for their area, discussed the challenges and strengths with reference to PPMD in their communities and made recommendations to address the challenges they face.
• Difficulty sleeping and eating
• Feeling lonely
• Irritability and frustration
• Feelings of guilt
• Tearfulness
• Feeling anxious and having panic attacks
• Constant worry
• Confusion
• Exhaustion
• Loss of joy
• Withdrawing from others
• Feeling like they are not bonding with their baby
If you have been experiencing any of these symptoms contact your local health card provider for more information. It is important to remember that you are not to blame for how you are feeling and you are not alone.
• asking for help
• talking to their doctor or nurse practitioner
• going to counselling
• getting out and attending Child and Family Centres
• talking to others about their experiences
• exercising
• drinking more water
• eating well
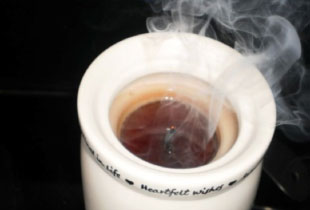
• limiting caffeine
• doing something for themselves each day
• challenging their own thoughts on being a “perfect” mother
If you have:
• had thought of harming your baby or yourself
• hear or see things that are not there
• believe people or things are going to harm you or your baby
• feel confused and out of touch with reality
Get help right away. Go to the Crisis Intervention Program at your local hospital.
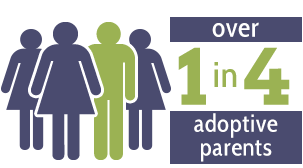
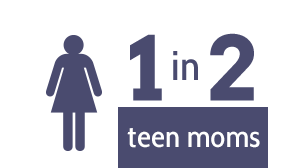
It is important to remember that not only mothers are affected by mood changes during and after pregnancy. Fathers and adoptive parents can also experience postpartum depression.
They can,
• ask her what she needs and fulfill those requests
• listen and support her
• help her understand it’s not her fault
• encourage her to access help
• spend time with your baby
• take care of yourself
• be patient

"I thought I must be the worst mother in the world to feel this way, to be sick like this, I thought my children would hate me for putting them through this, that I had screwed them up for life. But the truth was always reflected in their eyes, love was there not judgments, they just loved me the way I was. I could also see a light & hope in the eyes of my children that really helped motivate me to get help so I could and get better."
- Michelle Roberts

"This photo represents the time it took to find help. Although I was actively searching for help, waiting to get in to see my doctor and a counselor was senseless. Things are currently this way because of a lack of resources. Help should be available immediately for all who have realized they may be suffering from a PPMD. Currently, immediate help is available for those in crisis, but we need to be proactive so that a crisis is prevented. Mothers helping mothers. It also represents how I was just going through the motions of day to day activities and although the world continued around me, I felt that time was standing still. I have few memories of my children during this time. Although I tried to maintain normalcy in their lives, I was never really present in those moments."
- Sonia

"It felt like I was caught in turbulent seas, I couldn't see above the waves, it was a struggle to keep my head above water, it felt as if I was being pulled under, the wind was so high it knocked me down, I cried a sea of tears, and I began to panic as I was drowning in Postpartum Anxiety and Depression."
- Michelle Roberts
"This photo represents the moment when I lost myself. That my own light was extinguished. I felt myself slip into someone I didn't recognize. Feelings of hopelessness, anxiety, anger and fear. I was able to recognize the signs that depression and anxiety had overcome me. Prior to this, I was educated in what to look for and although others saw it before I did, I was able to seek help. Women and family members need to be educated to know the signs."
- Sonia

"When I finally admitted I needed help, I found that there are no direct services in my community for mothers & families who are suffering Postpartum Mood Disorders, There is a real gap in service for such a serious illness. Hopefully this project will bring those gaps to light and we can begin to fill them."
- Michelle Roberts

"Hold on... because this is going to hurt like hell". My husband was my rock. He was my life-saver and held on to me even as I was slipping away. He was my spine as he continued to hold our family together. He listened. He made me feel loved when I didn't think I deserved love. Family members need to have the education and support in how to handle all the feelings that may come with PPMD as well as the burden associated with holding a family together. It is important to know and understand that PPMD has a beginning, and it has an end. So hold on... until you get there."
- Sonia

"Stigma is defined as “a mark of disgrace associated with a particular circumstance, quality or person“. It is a negative stereotype. There is stigma associated with most mental illnesses, even PPMD. Many people view women with PPMD as weak, lazy, unable to handle the challenges of raising children. Some may think that a woman with PPMD is “ungrateful” for her family, that she “never should have had kids”; she is “just being selfish”. And, of course, she must be “crazy”.
Most communities can identify their local psychiatric units with a single word or expression, such as “the psych” in North Bay, “Kirkwood” in Sudbury, etc. During my illness, I did spend time admitted to hospital, “Riverview” being Sault Ste. Marie’s psychiatric unit at the time. Very few people came to visit me there, many unable to comprehend my illness. A few implied that I “just needed a break”, a rest from the daily grind of motherhood. They had no idea of the severity of my illness. I was removed from my children at a time when I most needed to feel connected to them. I told almost no one of the scariest thoughts and feelings I was having at that time for fear of being judged. I was afraid that I would be seen as an unfit mother, a threat, too unstable to be involved in my children’s lives.
Unfortunately, the stigma of mental illness prevents many from seeking the help that they desperately need as many are judged negatively by those around them. It takes great courage to talk about those intrusive thoughts, to admit that you’re worried you will harm your baby or yourself! By asking the difficult questions and acknowledging those scary, unpleasant thoughts without judgment, we can help women and families stay safe and become stronger. These moms need validation and reassurance that they are not “crazy”, not “monsters”, but that they have an illness that can be overcome. Friends and families need education about PPMD and how they can support the women and children in need of their help."
- Stephanie
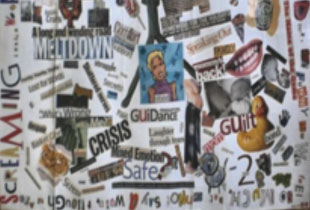
"This collage was created by me during my time in hospital. The images and words helped me to communicate my thoughts and feelings to my caregivers. Putting this collage together was a healing process as it helped me to identify and express how I was feeling.
I know that many women who have seen this collage can relate to some of the images. Women need to have a supportive network of other women with lived experience of Perinatal Mood Disorders to talk to. We must develop this network and make it as accessible as possible so that no mom ever feels alone."
- Stephanie

"Dreary, gray and lonely. For me, this picture represents my journey to wellness. There was no clear path to get there. I could only try to keep afloat until I hit solid ground. It seemed impossible to pick my way through the ever-changing maze while slowly sinking, allowing myself to melt into the cold silence. Each step forward was an unsteady leap.
We need to give women and families affected by PPMD a clear path to follow. They need help to navigate their way to solid ground. We need to support them on their journeys to wellness."
- Stephanie

"A mother’s mind is in a constant sway of firing neurons; full of overwhelming and uncontrollable emotions."
- Michelle

"Trudging through the cold, dark waters, fighting the way through the pressures of life and motherhood. Only to find that the light at the end of the tunnel is merely a continuing battle of river, feeling as though there is no end."
- Michelle

"Mothers often put their children’s needs before their own. Raising and carrying a child through life is an amazing but complex job. Mothers need to acknowledge and meet their own needs along with their family’s needs."
- Annie

"Becoming a new mother can be so overwhelming. Expectations and reality often collide leaving the new mother feeling disappointed, alone, misunderstood, guilty and lost."
- Annie

"When you’re drowning in post-partum fears and anxieties, there’s no trained expert to save you."
- Bonnie Dart

"When I desperately wanted information and support, I felt like I was left dangling, cut off from what I most needed."
- Bonnie Dart

"Post Partum Mood Disorder is a very frightening condition for those experiencing it as well as their family members. They need to know what it is, have a sense of what to do and what signs to look for."
- Bonnie Dart

"She is an isolated and unfamiliar "reflection". Alone she must navigate her way out of this deep, dense and dark place."
- Kathleen Jodouin

"This is not a minor pebble in her shoe. But she must carry this "monument" with her from now on."
- Kathleen Jodouin

"When I desperately wanted information and support, I felt like I was left dangling, cut off from what I most needed."
- Kathleen Jodouin

"What was needed most was a "break". Without relief from the pressure and stress of the experience she snapped."
- Kathleen Jodouin

"The sky was bright unlike my future. I felt like all I could do was cry and the tears would burst out of me so violently and so frequently. I felt all alone and out on an island where no one could reach me and a part of me didn't want to be reached. I didn't want people to know how bad I was. I was not me. I was someone else. Someone who was a failing at what was supposed to be the most natural role a woman could have. I was truly unworthy of such a title as mother."
- Janice Ireland

"It looked so peaceful and so inviting. I could walk in until the water slowly but steadily overtook my body and I disappeared. I would feel the cool water against all the searing pain of being a bad mother. I would welcome the water into my mouth and down my throat to soothe the rawness from all the sobs and I would let the water wash away all the tears from my cheeks. I would just disappear from this brutal and wretched life and no one would even miss me. How could they when I was already gone?"
- Janice Ireland

"A mother’s mind is in a constant sway of firing neurons; full of overwhelming and uncontrollable emotions."
- Janice Ireland

"During my pregnancy I had so many aspirations for what life would look like when our son was born. I had never expected that my experience with motherhood would be something I hadn’t prepared for; postponed until I could learn to find my identity again as a woman and mother after my post-partum depression swept in like a storm and left its heavy, cold presence on top of everything familiar and hopeful. Even throughout my recovery, much of that snow has remained as a thick blanket of guilt for being unwell in my son’s first few months. In my reflection of this experience, I have tried to figure out what could have helped to brush some of that snow away…and I see a need for women to speak openly and honestly about the transition and transformation that comes along with parenthood and to recognize that all change involves loss, and that loss looks different for every mother."
- Kaarina Ranta

"My depression encompassed many areas; anxiety, irritability, inability to leave my bed some days, crying spells, full blown outbursts, confusion and an overall feeling of chaos and nothingness . The bricks in the middle of the stream leading to the pool are meant to represent the barriers I had faced. As I started on my recovery journey, fluid and changing, like water, I had to learn to navigate through these barriers and find myself, unrecognizable on the other side of the bricks, joining the other women who had crossed over into motherhood, some with barriers and some without and learn who I was after this experience."
- Kaarina Ranta

"This photo is meant to depict how it felt to be in the middle of my illness. If the other side of the lake were to represent wellness, it is very far away. This woman is sitting alone and the tone is very cold and ominous, similar to my experience in that this was something I felt, and perhaps still do that no one could really understand the guilt, loneliness and embarrassment for not coping well. Trying to navigate the mental health services and identify what recovery was for myself was a very overwhelming task, exacerbated by lack of sleep and confusion, hidden to everyone except a close few. I would hope that the message people can take from this photo is that it is a very scary, unsure journey for a women to make and even if options are presented, it is a confusing time to assess what is needed and when to reach out."
- Kaarina Ranta

"This photo depicts how I think many mothers feel after they have gone through the exhaustive process of giving birth and they find themselves somewhat isolated in their motherhood and hanging on for dear life. The mountains in the photo help illustrate the peaks and valleys that many mothers can feel after delivering a baby and embanking on new motherhood whether it be for their first child or subsequent children."
- Mandy

"Mothers often judge themselves harshly and they certainly do not need more judgment from others when experiencing all the clashing emotions of post-partum life. It is critical that a mother's support system can move past judgment to seek understanding."
- Mandy

"A home away from home was what I needed when I was experiencing severe post-partum depression and my parents were graciously able to provide a welcoming, safe haven for myself, my husband, our toddler and our newborn daughter."
- Mandy

"Having children is overwhelming. Their needs overwhelm your needs and your thoughts. Their stuff overwhelms your house. Sometimes it feels like things will never be clear again."
- Christine Mackie

"The Journey through PPMD is like chasing rainbows. You know happiness is out there, but the closer you get the further happiness seems to get."
- Christine Mackie
"One of the hardest things to come to terms with is that sometimes you can`t be everything to everyone. Remember that kids are very resilient and forgiving. If only we could forgive ourselves."
- Christine Mackie
8 committees accross Northern Ontario came together tp create the Northern Ontario PPMD Strategy:
Country of origin:
Canada(Saskatchewan)
Action:
Recommendations
Education
Screening
Treatment
Sustainability & Accountability
Country of origin:
Australia
Action:
Strategies
Training & Workforce Development
Universal Routine Psychosocial Assessment
Pathways to Care
Country of origin:
New Zealand
Action:
Country of origin:
Canada(Ontario)
Action:
Recommendations
Service
Education and Training
Policy
Research
6 communiteis in Northeastern Ontario came together over the past year and created this strategy:
Addressing PPMD requires an investment in families. As PPMD impacts the entire family a partnership between the Ministry of Health and Long Term Care and the Ministry of Children and Youth Services is required. This invested collaborative partnership will provide a comprehensive continuum of care to families. This continuum of care will provide a menu of services for families and will utilize a variety of models of service delivery including electronic options that recognize the geographic challenges faced by those in the North. This model of care would be delivered in a person-centered, inclusive, holistic manner and would recognize the cultural diversity of the North and the diversity of familial connections. Services will be provided in a timely manner utilizing an expanded understanding of PPMD and will utilize inclusionary criteria rather than exclusionary criteria for admission.
×Provision of a system of care will require a coordinated system of competency building within our communities. This competency building should occur within all sectors that are involved with the provision of service and care to families and would respect the scope of practice of each sector. Systems of care include but are not limited to physicians, nurses, peer providers, social workers, early childhood educators, mental health and addiction workers, child protection workers, lay home visitors, psychotherapists, etc. Competency building would utilize best practice evidence related to PPMD in addition to the expertise of Northern communities of practice and Northern families with lived experience of PPMD.
×PPMD is an often an illness of secrecy, silence and shame. Upon the creation of a system of care and the enactment of a coordinated system of competency building we engage in a public education and awareness campaign. This campaign will utilize both traditional and non-traditional communication methods to provide accurate information on PPMD, pathways to care, and systems of support. This education will be provided in accessible and normalized language.
×Addressing PPMD requires an investment in families. As PPMD impacts the entire family a partnership between the Ministry of Health and Long Term Care and the Ministry of Children and Youth Services is required. This invested collaborative partnership will provide a comprehensive continuum of care to families. This continuum of care will provide a menu of services for families and will utilize a variety of models of service delivery including electronic options that recognize the geographic challenges faced by those in the North. This model of care would be delivered in a person-centered, inclusive, holistic manner and would recognize the cultural diversity of the North and the diversity of familial connections. Services will be provided in a timely manner utilizing an expanded understanding of PPMD and will utilize inclusionary criteria rather than exclusionary criteria for admission.
Provision of a system of care will require a coordinated system of competency building within our communities. This competency building should occur within all sectors that are involved with the provision of service and care to families and would respect the scope of practice of each sector. Systems of care include but are not limited to physicians, nurses, peer providers, social workers, early childhood educators, mental health and addiction workers, child protection workers, lay home visitors, psychotherapists, etc. Competency building would utilize best practice evidence related to PPMD in addition to the expertise of Northern communities of practice and Northern families with lived experience of PPMD.
PPMD is an often an illness of secrecy, silence and shame. Upon the creation of a system of care and the enactment of a coordinated system of competency building we engage in a public education and awareness campaign. This campaign will utilize both traditional and non-traditional communication methods to provide accurate information on PPMD, pathways to care, and systems of support. This education will be provided in accessible and normalized language.
×